Neuroendocrine Tumours – What You Need to Know about this Rare but Rising Cancer
Table of Contents
- What are neuroendocrine cells and neuroendocrine tumours?
- Types of neuroendocrine tumour
- Causes and risk factors of NET
- The incidence of neuroendocrine tumours in different locations
- The signs and symptoms of neuroendocrine tumours
- How to diagnose neuroendocrine tumours
- Stages, grades, and prognosis of neuroendocrine tumour
- Treatment of neuroendocrine tumour
- How to prevent NET cancers
- Takeaway message
Table of Contents
- What are neuroendocrine cells and neuroendocrine tumours?
- Types of neuroendocrine tumour
- Causes and risk factors of NET
- The incidence of neuroendocrine tumours in different locations
- The signs and symptoms of neuroendocrine tumours
- How to diagnose neuroendocrine tumours
- Stages, grades, and prognosis of neuroendocrine tumour
- Treatment of neuroendocrine tumour
- How to prevent NET cancers
- Takeaway message
Neuroendocrine tumours (NETs) are a rare but diverse type of cancer originating from neuroendocrine cells, which are found all over the body. Though relatively uncommon, the incidence of neuroendocrine tumour is increasing all over the world. A similar rise is seen locally, with recent research showing an almost fourfold increase in the number of reported NET cases over the last two decades in Singapore.
In this general guide to neuroendocrine tumours, we will cover the essentials you need to know about this cancer, including their causes, symptoms, types, prognosis and treatments. First, let us start with the basics – what are neuroendocrine cells and neuroendocrine tumours.
What are neuroendocrine cells and neuroendocrine tumours?
Neuroendocrine cells, as the name suggests, play the dual functions of being both neurons and endocrine cells. Their role is to produce and release hormones into the bloodstream upon getting the instructions from the brain.
Neuroendocrine cells are scattered throughout the body but can mostly be found in the gastrointestinal tract, pancreas, gallbladder, thyroid, lungs and respiratory tract. The hormones generated by neuroendocrine cells help with various bodily functions, such as digestion, metabolism, regulation of blood sugar, blood pressure and heart rate.
Neuroendocrine tumours (NETs) form when these neuroendocrine tissues turn cancerous and do not carry out their functions properly. They may start releasing hormones in an uncontrolled manner or stop making sufficient hormones, both of which can lead to devastating consequences.
A few years back, researchers classified neuroendocrine tumours into cancerous and noncancerous. However, this is not the case anymore. Today, all neuroendocrine tumours are considered cancerous.
Types of neuroendocrine tumour
Functional vs nonfunctional NETs
There are several ways to classify neuroendocrine tumours. However, it is important to differentiate between functional and nonfunctional NETs, as treatment protocol depends on whether the tumour is functional or not.
Functional tumours refer to NETs that produce excess amounts of hormones. Conversely, nonfunctional tumours may produce little to no hormones. Depending on the type of tumour, the specific hormone that is being secreted is different. According to the American Society of Clinical Oncology (ASCO), around 60% of NETS are nonfunctional.
Types of NETs by primary tumour site
Aside from functional and nonfunctional NET, neuroendocrine tumours are also classified by the primary site they originate from. The main groups include:
- Gastroenteropancreatic neuroendocrine tumours (GEP-NETs): Starting along the digestive tract, GEP-NETs can be further classified into subtypes, including:
- Stomach NETs
- Small bowel NETs
- Large bowel and rectum NETs
- Pancreatic endocrine tumours (PETs)
- Lung NETs: Developing in the neuroendocrine cells of the lungs. Depending on the types of cells that cancer, we have 4 main subtypes of lung NETs
- Small cell lung cancer (SCLC)
- Large cell neuroendocrine carcinoma (LCNEC)
- Typical carcinoid
- Atypical carcinoid
- Merkel cell carcinoma: This tumour starts in a type of neuroendocrine cells most often found in the skin called the Merkel cells.
- Others: NET of the thyroid gland (Medullary thyroid carcinoma), NET of the thymus (NETTs)
Carcinoid tumour vs. neuroendocrine carcinoma
Some types of NET are also referred to as carcinoid tumours. Generally speaking, carcinoid tumour refers to a slow growing NET. These cancers can affect the neuroendocrine cells in the lung or pancreas. They typically have well-differentiated cells, which means they look normal under the microscope.
On the other hand, neuroendocrine carcinoma describes a high-grade NET. Despite how rare neuroendocrine carcinomas are, they can be very aggressive.
Causes and risk factors of NET
So far, there is no definitive evidence of what exactly causes neuroendocrine tumour. Additionally, a majority of cases develop in people with no family history of NETs.
Identified risk factors include some genetic syndromes. These conditions develop in people who get the gene from one of their parents and may increase the risk of NETs. They include:
- Multiple endocrine neoplasia type 1
- Von Hippel-Lindau disease
- Tuberous sclerosis
- Neurofibromatosis type 1
Certain medical conditions can also increase the odds of developing NET. For instance, people who have a low rate of acid production in the stomach are thought to have a higher risk of NETs.
Note that advanced age is not a risk factor for developing NET, though researchers tend to think that it affects prognosis and treatment outcomes. In Singapore, one in three cases of NET is diagnosed under the age of 50.
The incidence of neuroendocrine tumours in different locations
NETs can develop in several organs in the body. However, we see the vast majority of cases in the digestive tract. After the GI tract, the lungs commonly host NETs, followed by the pancreas.
Here is a breakdown of NET’s incidence by primary tumour site, based on a recent study of NET in Singapore:
- 7% in the stomach
- 6% in the small intestine
- 14% in the large intestine (colon)
- 26% in the rectum
- 14% develop in the lung and bronchus
- 9% in the pancreas
- 24% in other organs or unknown

The signs and symptoms of neuroendocrine tumours
NET cancer symptoms are usually absent during the early stages of cancer. The lack of early symptoms allows the tumour to grow in silence without being detected over many years, often until it reaches a certain secretion rate or size that causes clinical symptoms. Even when the cancer is advanced, the symptoms vary widely from one type to another, depending on factors such as:
- The original site of the tumour and the endocrine gland it affects
- The size of the tumour
- Whether it is a functional or non-functional tumour
- Whether NET has metastasized to other parts of the body
Generally speaking, we can classify the symptoms of NET into two types:
Hormonal symptoms – This is the result of excess hormone production. Such symptoms include fluctuating blood sugar levels, diarrhoea, and gastric ulcers.
Mechanical symptoms – When the NET cancer becomes large enough, it places physical pressure on the nearby organs. For instance, a NET cancer of the digestive tract may lead to bowel obstruction, causing symptoms such as abdominal pain or cramp, constipation, vomiting, difficulty passing motion, etc.
Unfortunately, the absence of specific symptoms in NET often results in delayed diagnosis and thus compromises in treatment outcomes.
How to diagnose neuroendocrine tumours
If it is often after the other causes have been ruled out for the hormonal or mechanical symptoms that a patient is referred to an oncologist or specialist with suspicion of NET. The diagnosis of a neuroendocrine tumour requires going through the following steps:
Taking your medical history – Your doctor will ask you questions about your current symptoms and previous conditions.
Performing a physical exam – Once your doctor completes your medical history, he/she will perform a comprehensive physical examination to determine the impact of your NET cancer on your functions.
Ordering a few biological tests – Biological tests are crucial to objectify the levels of the affected hormones. For instance, NET cancer affecting the adrenal glands leads to excess production of epinephrine.
Ordering imaging tests – Imaging tests, such as ultrasound, CT scans, and MRI, can help locate your NET cancer. The most effective imaging test to visualise NETs is often positron emission tomography (PET).
Performing a biopsy – Collecting a tissue sample and sending it to the pathology lab can give the oncologist extensive information about your NET cancer. There are several procedures that allow your doctor to collect the sample, including bronchoscopy (for lungs), gastroscopy (for oesophagus and stomach), and colonoscopy (for rectum). If the tumour is located in an inaccessible area, surgery may be necessary to collect the tissue sample.
After collecting information from all of these steps, your doctor will be able to confirm the diagnosis of the NET cancer and determine the type that is affecting you.
Stages, grades, and prognosis of neuroendocrine tumour
Staging and grading NETs helps doctors classify the characteristics of the tumours and better determine treatment for their patients. Due to the heterogeneous nature of this cancer, there is no single system to stage NETs. However, NET grading is simpler, often consisting of:
- Grade 1: Considered a low-grade tumour, grade 1 NET often grows slowly.
- Grade 2: Also known as intermediate grade tumour, NET grows at an intermediate rate.
- Grade 3: This high-grade cancer is known to be aggressive with the tumour growing quickly.
Many patients want to know their prognosis based on the stage and grade of the tumour. It is possible for the doctor to provide an indication of recovery chances, commonly known as prognosis or outlook, based on past data of people having the similar tumour stage and type. The most common metric is the 5-year relative survival rate.
The table below demonstrates historical survival rates of neuroendocrine tumours, according to an epidemiological study of neuroendocrine tumour in Singapore.
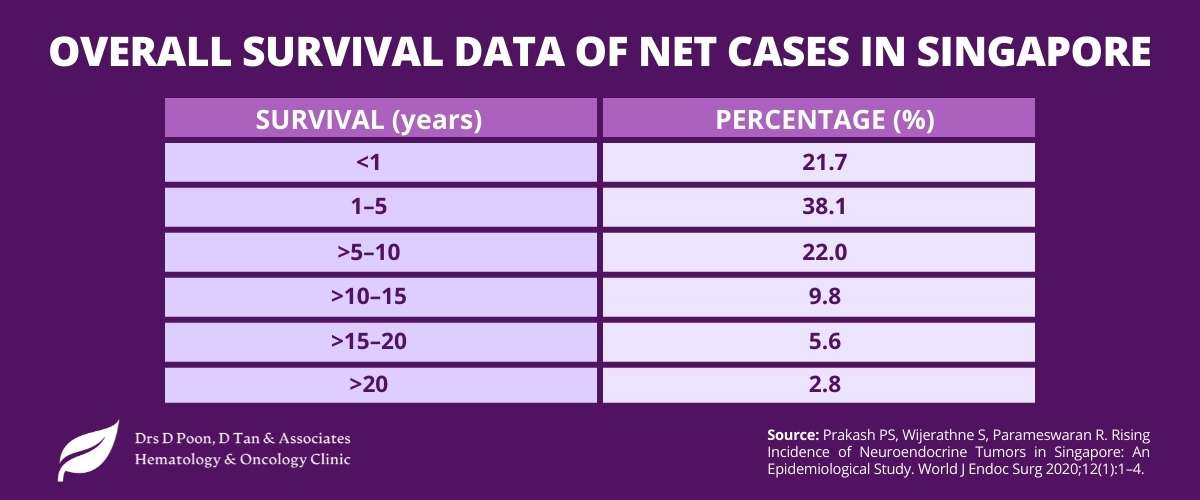
Note that these calculated rates do not consider the age, health status, and cancer response to treatment, and thus, should be taken with a grain of salt. Besides, the past survival rates may not necessarily come true in the future. This is because treatments are constantly improving, which enhances the chance of recovery.
Make sure to discuss your case with your doctor to determine the best and most effective treatment protocol to improve the outlook of your NET cancer.
Treatment of neuroendocrine tumour
As neuroendocrine tumours are diverse, treatment varies greatly, depending on the type, stage and grade of NET you have. Other factors, such as location, symptoms, and level of hormone secretion, also affect the type of treatment you receive.
Unlike other types of cancer, the medical professionals who treat NETs may have different specialties based on the location of the tumour. For instance, if you have pancreatic NET, you may need to consult an oncologist specialising in gastrointestinal tumours.
Depending on the characteristics of your NET, cancer may be treated by one or more of these specialists:
- Endocrinologists
- Gastroenterologists
- Pathologists
- Surgeons
- Medical oncologists
- Transplant specialists
- Radiologists
- Nuclear medicine specialists
To address NET cancers, the doctors may recommend one or a combination of the following common treatments:
Surgery
Surgery is effective at removing the tumour when possible. If the tumour is accessible, your surgeon will remove the entirety of the cancerous neuroendocrine cells, along with some healthy tissues. If this is not possible, the surgeon will try to remove as much of the tumour as possible. This treatment is often recommended for NET that is localised. However, surgery comes with its own risks and therefore might not be suitable for all patients with early stage NET.
Chemotherapy
Chemotherapy is a common treatment for NET cancers. These drugs are powerful enough to destroy the rapidly-growing cells of the tumour. Your doctor may recommend chemotherapy through your vein or as an oral medication.
To lower the risk of cancer recurrence, your oncologist may prescribe post-surgery chemotherapy. Advanced NET cancers with no hope of surgical removal also benefit from chemotherapy.
Targeted drug therapy
Targeted drug therapy works by focusing on specific physiological features of the neuroendocrine cells. Blocking these abnormalities leads to the death of these cells. Combining chemotherapy with targeted drug therapy can create a powerful treatment protocol.
Peptide receptor radionuclide therapy (PRRT)
Peptide receptor radionuclide therapy, or PRRT, focuses on treating cancer cells by combining a drug with a small amount of radioactive substances. This allows the radiation to reach the cancerous cells.
A classic example of a PRRT drug is lutetium Lu 177 dotatate (Lutathera), which is very helpful in treating advanced cases of NET cancers. Some side effects of PRRT include nausea, vomiting, edema (i.e., swelling), belly pain, and temporary hair loss.
Hormonal therapy
Your neuroendocrine tumour may be functional and release excess hormones. To combat the symptoms that stem from this disturbance, your doctor might prescribe hormonal medications.
For instance, a type of drug called somatostatin analogues has shown positive results in treating carcinoid syndrome in pancreatic NET. It works by mimicking the body’s natural somatostatin and regulating the body’s hormonal production.
Radiation therapy
Radiation therapy uses energy beams to kill the NET cancer. This option is not always ideal for all types of NETs. It is most helpful when surgery is no longer an option.
How to prevent NET cancers
Unfortunately, there is no definitive way to completely prevent neuroendocrine tumours. For instance, there is nothing you can do if you have a family history of NETs. Additionally, the vague causes and risk factors of NET cancer make us unable to prevent these tumours.
With that said, maintaining a healthy lifestyle is known to reduce the risk of cancer in general, as well as many other medical conditions. If you have a risk factor or family history of a specific type of NET cancer, speak with your doctor about the best preventive measures to lower your prospective risk.
Going for health screening regularly also helps with early detection of NET cancer, which can enhance treatment effectiveness. The most common type of NET – NET of the GI tract – can be discovered with a gastroscopy and colonoscopy, the same procedure that is used to screen colorectal cancer. Speak to your gastroenterologist about your risk or find out how you can make use of the government-subsidised colorectal screening program in Singapore and check out our article on how to make the most use of cancer screening here.
Takeaway message
Despite being a rare type of cancer, neuroendocrine tumours are challenging due to the absence of symptoms in the early stages, delayed diagnosis and thus, compromised treatment outcome. Another concern is the rising incidents of NET in Singapore, the causes of which are not fully understood.
We hope this article provides the essential knowledge of this type of cancer, helping you to better manage its risk for yourself or a loved one. Knowledge helps with early detection, and early detection can save life.
Dr Donald Poon